April 2018 | Resource
The next generation of health IT spend: A tactical guide
A prescriptive approach to right-sizing your hospital or health system’s IT investment profile based on your strategic priorities
In The Next Generation of Health IT Spend, we summarized the recent history of health system technology spend and provided a point of view on where the trend is headed. Additionally, we proposed a new set of technology investment portfolios based on a health system’s mission and vision for future growth. We also delineated areas and levels of financial investment required to match their desired investment profile.
However, many struggle to define the investment profile that makes the most sense for their organization. In this guide, we present a prescriptive method for planning your technology spend portfolio to be a lever for competitive differentiation as well as a value generator for your system and the communities you serve.
Quick refresher and overview
In The Next Generation of IT Spend, we discussed recent market trends affecting health systems, how health systems can think about technology as an investment profile, and what the future holds for technology spend.
Following the two “Mass Scrambles” that were driven by the American Recovery and Reinvestment Act (ARRA) in 2009 and Meaningful Use requirements, the industry saw a significant increase in technology spend. Currently, hospital executives are left with ambiguity around technology investments.
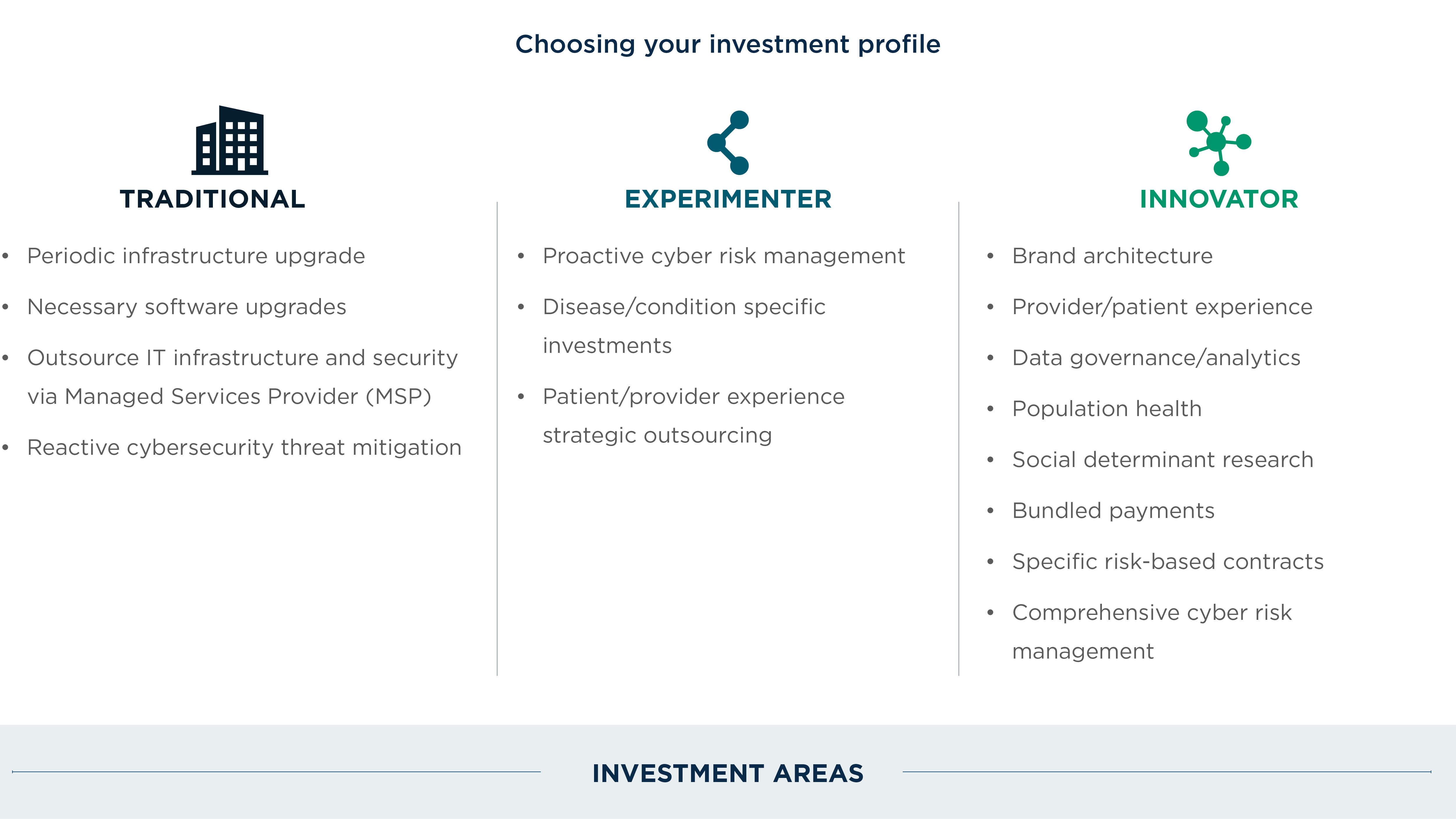
Multiple forces at play, including cybersecurity threats and reimbursement pressures, indicate there is no relief in sight for IT spending. However, a prescriptive strategic investment band can help guide spending decisions in a way that aligns IT spend with business and community strategies. Health systems will ultimately fall into one of three categories: traditional, experimenter, and innovator. In this paper, we will outline a prescriptive approach to right-sizing your hospital or health system’s IT investment profile based on your strategic priorities. (Complex industry forces are demanding that health systems reassess their technology strategy.) Market forces like consumerism, reimbursement pressures, a changing regulatory environment, aging populations, the supply and demand gap, and threats to data security are challenging health systems to reconfigure their technology investment profile. To understand how technology can help combat these forces, organizations must right-size their IT budgets to meet the demands of new strategies.
Chapter 1: Developing the current state
Every health system has capabilities (of varying maturity) that are vital to keeping operations running but also in mitigating the challenges posed by current market forces. Each of these capabilities is achieved through a combination of people, processes, and technology.
Understanding the strengths, gaps, and priorities of your organization is critical for making investment decisions.
When doing so, health systems should evaluate themselves against what the hospital system of tomorrow will be, not necessarily against their peers of today. A significant amount of legacy IT is likely to exist across your organization, so be prepared for an investigatory process.
Chapter 2: Target operating model
After understanding the current state of the organization, the next step is to understand where you want to go. This does not mean that every health system should strive to achieve the highest level of maturity in every aspect of their business; it is a matter of right-sizing the various maturity levels to effectively support established business and community strategies. At each juncture, it is critical to ask the following value questions:
- Will the desired degree of future state maturity in a defined area (e.g. application portfolio, data governance) create value? How will we capture the value created?
- How do we define value in the context of security? What is our governance model for security? How do we collaborate between the technology team and security officers?
- Which areas of our business are candidates for outsourcing operations or technology? What is the value delivered through outsourcing? Operating margin, flexibility, speed to market?
- What is the time horizon for us to capture value? What are alternative ways to achieve the same value through other means (such as partnering with a technology vendor, another health system, payers, etc.)?
- What intangible value can be created and/or captured by the future state maturity? How do those support our mission, vision, and community standing? What is our strategy as it relates to cloud, data center, and self-hosted applications? What value are we obtaining from this strategy? What is the business case for going to the cloud?
- Are the investment levels justified for the maturity improvement in all areas?
Chapter 3: Building a pragmatic roadmap
A natural outcome of the Target Operating Model is a set of fact-driven gaps—the distance between the current state and what the target-state maturity model outlines. The fulfillment of these gaps is essentially the roadmap to achieving the desired future state.
Most well-intentioned strategy projects end up as documents on a shelf, rarely utilized or used to execute. This phase must not result in a typical roadmap—a directional, high-level category of improvement areas and rough, ballpark dollar estimations. Such high-level roadmaps are a sure way to never make real change.
The fact is that health systems have more projects that they should do than they can do, especially in technology. The question is which projects will you commit to in order to make the roadmap a practical tool of execution that is prioritized, sequenced, and resource-conscious. This roadmap should be used to hold technology leaders and business sponsors accountable in creating and capturing value.
A strategic reporting mechanism (dashboard, board-level summary of key metrics) must be identified to visualize and track the progress along the roadmap. As in the Target Operating Model, the value framework needs to be used to identify value created and value captured through each project or initiative on the roadmap. The value framework will help prioritize the projects in the order they should be executed or how they should be dealt with in case of a triage. Additionally, tie the strategic business and community objectives of the larger organization to each project so as to provide a narrative value for each project.
The fact is that health systems have more projects that they should do than they can do, especially in technology. ”
Lastly, a thorough analysis must be done to estimate the effort hours, types of resources, one-time costs inclusive of software, hardware, implementation costs (whether internal labor or external), and ongoing costs. All existing projects in flight should be consolidated in this list. The detailed roadmap must be iterated upon multiple times with both business sponsors and technology leaders until it becomes part of the culture.
Conclusion
First, understand the current state of your organization’s strategy, capabilities, and budget. Then, determine what your future state should look like in a reasonable way. Finally, develop a pragmatic roadmap, one that you will use to hold your own leadership accountable.